Embarking on a surrogacy journey is an act of love, courage, and hope. From choosing your agency to building trust with your gestational partner, to nurturing every step leading up to your first embryo transfer — so much emotional energy goes into that moment. When that first transfer doesn’t result in a pregnancy, it can feel devastating. It’s natural to grieve, to worry, and to question what comes next.
But here’s the truth, supported by both data and clinical experience: a firstattempt embryo transfer failure is very common, medically expected for many, and often just one turn on the path toward building your family. This experience does not mean your dream is fading — it means your journey is unfolding in the way it has for countless successful parents before you.
First, Let’s Normalize This Experience
Even with highly screened gestational carriers and top-quality embryos, not every embryo will implant on the first try. Reproductive medicine is an incredible science, but it is still influenced by many variables that are beyond absolute control.
Across IVF and surrogacy programs, many intended parents find that it takes more than one embryo transfer to achieve pregnancy, meaning the first attempt may not succeed — and still be within normal outcomes.
Implantation is one of the most complex biological events in medicine and even excellent embryos can fail to implant for reasons that are simply outside current science’s full understanding.
It’s okay to feel disappointed. It’s okay to question what happened. But it’s also important to know: this is a setback, not destiny.
Why Might a First Transfer Not Work?
When intended parents hear that “the transfer didn’t take,” it’s natural to search for a single explanation. However, the reality is that multiple factors influence implantation — and often none can be pinpointed as a sole cause.
Embryo competence
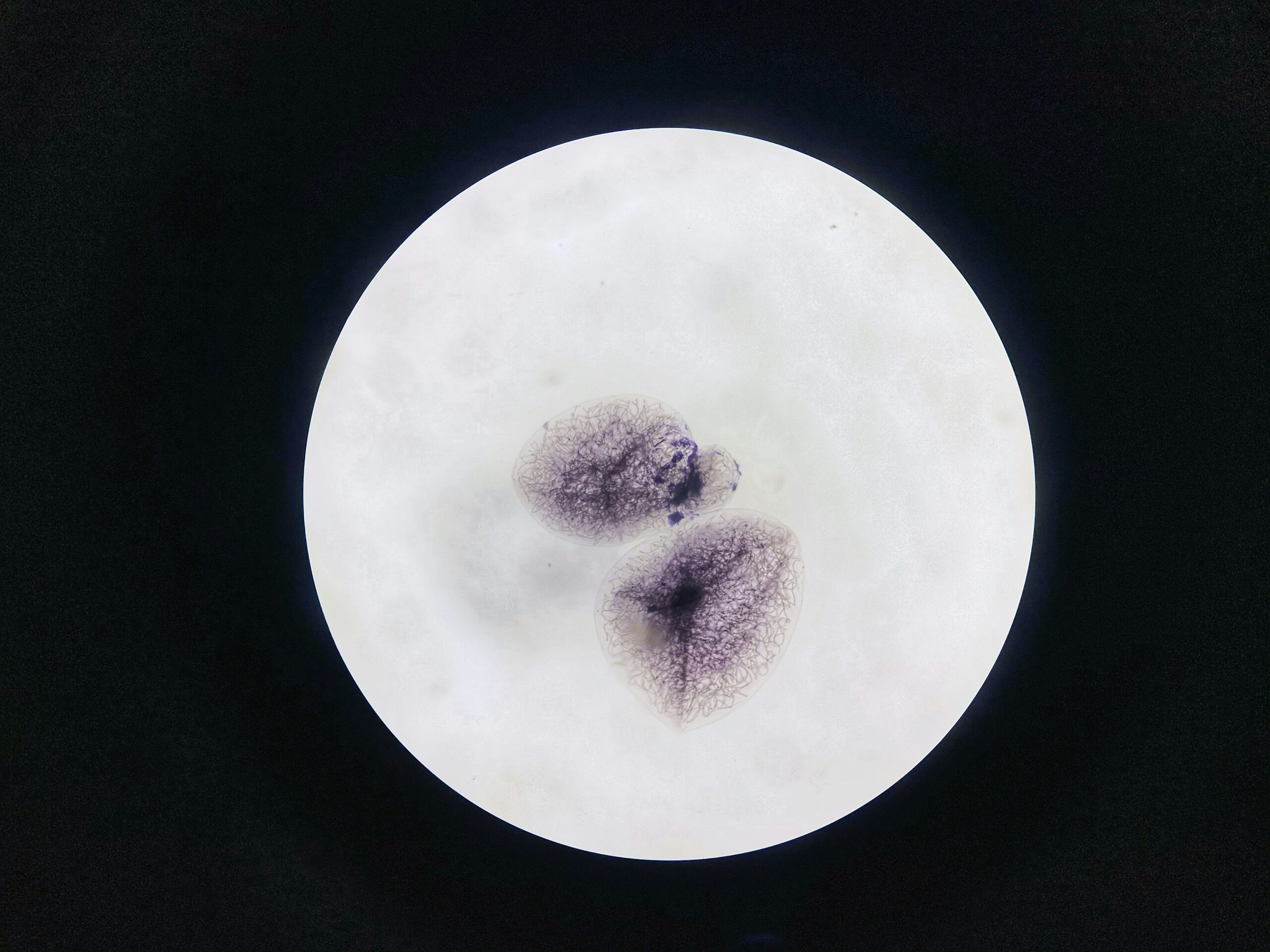
Even highly graded and genetically tested embryos (such as those screened with PGT-A) can fail to implant because implantation requires a highly orchestrated interaction between embryo and uterus. Many embryos, even those that look healthy under the microscope, have chromosomal abnormalities that prevent implantation or early development. Research shows that most embryos naturally stop developing shortly after fertilization due to spontaneous errors in early cell division.
Endometrial timing and synchronization
Successful implantation requires perfect timing between the embryo and the uterine lining. If the endometrium isn’t precisely receptive, even by a matter of hours, the embryo may not implant. Subtle mismatches in molecular signaling or uterine receptivity – which are out of everyone’s control and ability to mitigate – can prevent implantation, even in perfectly healthy surrogate carriers.
Hormonal and immune environment
Subtle hormonal fluctuations or immune responses, even in perfectly screened and healthy surrogate carriers, can influence implantation success.
Clinic protocol variations
Clinics continually refine protocols based on real-time results. Sometimes the first cycle yields insights that help optimize the next one – fine-tuning medication timing, hormone support, or transfer scheduling.
These aren’t “mistakes” or signs of failure. They are reminders of how intricate human biology is.
Success Beyond the First Try
It helps to see the bigger picture. While many first embryo transfers do not lead to a live birth, the chances of success rise with multiple attempts:
Analyses show that cumulative live birth rates increase significantly with subsequent transfers: approximately 65% after the first transfer, ~84% after the second, and over 92% after the third for chromosomally normal embryos (Embryoman, 2021).
What Happens Next?
After an unsuccessful transfer, your medical care team doesn’t simply “try again.” Instead, they review with care. Your specialists may recommend:
- Adjusting medications
- Trying a slightly different protocol
- Evaluating the timing window more closely
- Transferring another embryo
- Additional supportive testing if medically appropriate
- No change at all
- Switching surrogate partners
Every step forward becomes more informed because of what this first attempt taught the team.
Self-Care in This Moment
This experience is more than medical – it’s deeply emotional. Many intended parents describe a first failed transfer as a grief moment…grieving the vision they had, the timeline they hoped for, the “certainty” that they felt they should have by then.
Here are gentle reminders as you process this:
- Your emotions are valid. Sadness, frustration, fear, hope — they can all coexist.
- You did not fail. You are actively pursuing parenthood with courage.
- Your gestational carrier did not fail. She is in this journey with you, and compassion matters.
- This moment doesn’t define your future. Success often comes after learning from what didn’t work.
- You’re not alone. Your agency care team and support network are with you.
Consider talking through your feelings with supportive professionals, joining communities of intended parents who’ve walked this path, and giving yourself permission to take the time you need to process.
Hope and Success
Here is the part we want you to hold close:
- A failed first transfer often precedes a successful one.
- Many families who faced this very moment went on to welcome healthy babies.
Surrogacy is built on hope, science, compassion, and resilience. A first embryo transfer that doesn’t result in pregnancy may feel heavy — but it does not erase your future, your strength, or your dream of parenthood.
This isn’t the end. It’s a chapter in your story — one that many parents have lived through before standing where you hope to stand. You are seen. You are supported. And there is every reason to believe your dream of holding your child is just on the horizon.